Background: Percutaneous laser disc decompression (PLDD) for patients with lumbar disc herniation is believed to be cheaper than surgery. However, cost-effectiveness has never been studied.
Materials and Methods: A cost utility analysis was performed alongside a randomized controlled trial comparing PLDD and conventional surgery. Patients reported their quality of life using the EuroQol five dimensions questionnaire (EQ-5D),
36-item short form health survey (SF-36 and derived SF-6D) and a visual analogue scale (VAS). Using cost diaries patients reported health care use, non-health care use and hours of absenteeism from work. The 1-year societal costs were compared with 1-year quality adjusted life years (QALYs) based on the United States (US) EQ-5D. Sensitivity analyses were carried out on the use of different utility measures (Netherland (NL) EQ-5D, SF-6D, or VAS) and on the perspective (societal or healthcare).
Results: On the US EQ-5D, conventional surgery provided a non-significant gain in QALYs of 0.033 (95% confidence interval (CI) _0.026 to 0.093) in the first year. PLDD resulted in significantly lower healthcare costs (difference E1771, 95% CI E303 to E3238) and non-significantly lower societal costs (difference E2379, 95% CI _E2860 to E7618). For low values of the willingness to pay for a QALY, the probability of being cost-effective is in favor of PLDD. For higher values of the willingness to pay, between E30,000 and E70,000, conventional microdiscectomy becomes favorable.
Conclusions: From a healthcare perspective PLDD, followed by surgery when needed, results in significantly lower 1-year costs than conventional surgery. From a societal perspective PLDD appears to be an economically neutral innovation.
Introduction
Microdiscectomy is the most frequently performed surgical procedure for patients with sciatica caused by lumbar disc herniation. This open surgical treatment approach is aimed at the removal of the herniated disc fragment causing nerve root compression.
Another indirect way of decompressing the compromised nerve root is by reducing the pressure in the intervertebral disc by removal of herniating disc material.
Several percutaneous techniques are based on this principle, including percutaneous laser disc decompression (PLDD). An attractive feature of PLDD is its minimally invasive nonsurgical nature. In a randomized clinical trial, we compared PLDD with conventional microdiscectomy in a subgroup of patients. The trial showed that a strategy of PLDD only followed by surgery when needed, in patients with sciatica due
to a lumbrosacral disc herniation, was not inferior to open surgery at 1 year at the cost of higher retreatment
rates and a longer time to recovery. PLDD is associated with lower short-term healthcare costs than conventional surgery, as it does not require hospitalization and anesthesia. To date no economic evaluations comparing PLDD with surgery have been performed, therefore cost-effectiveness of PLDD is yet to be established.
We carried out a cost utility analysis of our randomized controlled trial, comparing observed 1-year quality adjusted life years (QALYs) with observed 1- year societal costs to determine whether favorable osteffectiveness for a strategy of PLDD is attained over a direct surgical strategy approach.
Methods
Patients with sciatica due to nerve root compression lumbar disc herniation participated in a multicenter randomized controlled trial that compared conventional microdiscectomy with PLDD. Institutional Review Boards of participating hospitals approved the research protocol and participants gave written informed consent. A total sample size of 110 was chosen, based on equality in effect on the Roland Disability Questionnaire for Sciatica (RDQ) between microdiscectomy and PLDD. Between January 2005 and September 2007, 115 patients were enrolled and 112 patients were analyzed (55 patients were allocated
to PLDD and 57 to surgery). Overall, three patients were excluded after randomization, two withdrew
before treatment and one was excluded before treatment because of protocol violation. Both groups were
comparable regarding their baseline characteristics.
Patients and treatment
Eligible patients were between 18 and 70 years old with a radiologically confirmed disc herniation and corresponding lumbosacral radicular syndrome lasting more than 6–8 weeks. The herniated fragment had to be smaller than 1/3 of the spinal canal. We excluded patients with cauda equina syndrome, previous spinal surgery at the same disc level, spondylolisthesis, bony spinal stenosis, pregnancy, severe somatic or psychiatric diseases, inadequate knowledge of Dutch language, or emigration planned within 1 year of inclusion.
The details of treatment can be found elsewhere. Briefly, microdiscectomy was performed by an ipsilateral
approach with midline paravertebral muscles retraction and herniated disc removal by a transflaval approach without or with minimal bone removal.
Surgery was finished after the nerve root decompression was visible and loose disc fragments removed.
In case of PLDD, laser energy is delivered via an optical fiber delivered through an 18G needle placed
into the nucleus pulposus via a posterolateral approach. In contrast with other minimally invasive surgical procedures this treatment is performed under local anesthesia, not requiring an anesthesiologist. As a
result of the laser disc decompression, in which water content of the nucleus pulposus is decreased due to
vaporization, the herniated disc will shrink, which will result in a reduction in nerve root compression.
Utilities and QALYs
Utilities represent the valuation of the quality of life of the patients, anchored by zero (as bad as death) and
one (perfect health). Patients described their quality of life using the EuroQol classification system (EQ-5D),
from which we calculated utilities for the United States (US) and The Netherlands (NL). Similarly, patients reported their quality of life using the 36-item short form health survey (SF-36), from which we calculated the SF-6D utilities.6 Both EQ-5D and SF-6D provide societal valuation, which is preferred for economic evaluations from a societal perspective. In addition, we obtained valuations by the patients themselves, using a visual analogue scale (VAS) ranging from 0 (worst imaginable health) to 100 (perfect health). We transformed the values to a utility scale, using the power transformation 1_[1_VAS/100].
We obtained measurements for EQ-5D and the VAS at randomization and 3, 4, 6, 8, 12, 26, 38, and 52 weeks after randomization. SF-36 measurements were obtained less often; at randomization and 4, 8, 26,
and 52 weeks after randomization. For the EQ-5D, SF-36 and VAS measurements, respectively 5%, 9%
and 6% of the items were missing. From the area under the utility curves we calculated the average utility
during each separate quarter of the year after randomization and during the entire year (QALYs).
Costs
We estimated the costs from the societal perspective during the 1 year of follow up. Because of the 1-year
time horizon, costs were not discounted. Costs were converted to 2010 price levels using the general Dutch consumer price index.
Using cost diaries, patients reported admissions to hospital, visits (specialists, general practitioner, physical
therapy, and alternative health care), homecare, paid domestic help, informal care, drugs and aids, out of pocket expenses as result of the sciatica, and hours of absenteeism from work.
At the follow up at 4, 8, 26 and 52 weeks after randomization the research nurse went through the diary with the patient. At these follow-up intervals, 2%, 2%, 3% and 7% of the diaries were missing respectively.
Integral costs of surgery were based on cost prices of participating hospitals. Costs of surgery were estimated at E2428 excluding hospital stay. Integral costs of PLDD were estimated at E868 based on a microcost calculation of direct and indirect personnel, equipment, material, and overhead costs for the treatments. For scheduled treatments that were cancelled at the last moment (for example because of recovery of the patient) costs of personnel and equipment, and overhead costs were included (as no other intervention could be scheduled) but no cost of consumables.
For other health care, we used Dutch standard prices, designed to represent societal costs and to tandardize
economic evaluations.
Health care costs are reported including the patients’ time and travel costs.
We valued the reported hours of absenteeism from work and hours worked less in the case of a decrease in working hours during the 1 year follow-up period according to the friction cost method using a friction period of 22 weeks,9 at standard productivity costs of E34 per hour for women and E43 per hour for men.
Analysis
All analyses followed the intention to treat principle. All statistical analyses were conducted with Stata version 9.2 (StataCorp, College Station, TX, USA).
To reduce possible bias due to missing data, we used multiple imputation by chained equations,10 with five
iterations for the switching regression model. For each missing utility measure or cost measure, an imputation regression model was used that included the patient’s age, sex, body mass index, randomization group, patient’s reported functional disability measured by the Roland Disability Questionnaire for Sciatica, VAS for leg and back pain, duration of complaints, and all (other) utility measures and costs measures at all (other) moments.
Group differences in QALYs and costs were statistically analyzed using standard unequal-variance Student’s t-tests.
Base case cost utility analysis compared 1-year societal costs with 1-year QALYs based on the US EQ-5D.
Sensitivity analyses were carried out on the use of different utility measures (NL EQ-5D, SF-6D, or VAS) and
on the perspective (societal or healthcare perspective).
Depending on the willingness to pay for obtained effectiveness, a strategy is cost-effective compared with an alternative strategy if it has a better average net benefit [willingness to pay _ QALYs _ costs].
Acceptability curves are constructed, in which the y-axis represents the probability that PLDD is costeffective
compared with conventional microdiscectomy.
The value 0.5 represents equality in cost-effectiveness between two treatments, based on the amount of
money (threshold) society is willing to pay per QALY. In Figure 1, PLDD can therefore be considered cost-effective if the value exceeds 0.5 for a given willingness to pay.
Results
Utilities and QALYs
According to the EQ-5D the valuation of quality of life for PLDD 2 weeks after randomization was better than
for surgery (Figure 2). However, after that time the utility measures were consistently worse for PLDD than for surgery. The VAS and the SF-6D provided similar pictures, although the quality of life of PLDD patients according to the SF-6D was better until 8
Figure 1. Cost-effectiveness acceptability curves for PLDD compared with conventional microdiscectomy
EQ-5D: EuroQol five dimensions questionnaire; NL: Netherlands; PLDD: percutaneous laser disc decompression: QALY: quality adjusted life
year; US: United States
Figure 2. Utilities (including confidence intervals) according to US, NL EQ-5D, SF-6D, and VAS
CD: conventional discectomy; EQ-5D: EuroQol five dimensions questionnaire; NL: Netherlands; PLDD: percutaneous laser disc decompression;
SF-36: 36-item short form health survey; US: United States; VAS: visual analogue scale.
weeks after randomization, while according to the VAS the quality of life of PLDD patients were only better at
8 weeks.
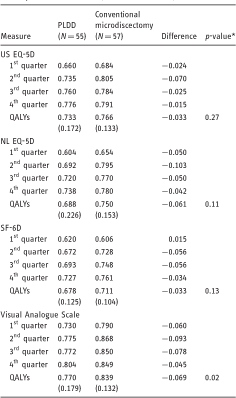
Utilities during all four quarters and according to all measures were consistently less favorable after PLDD,
except for the first quarter according to the SF-6D (Table 1). The largest difference in utilities was observed in the second quarter, 0.103 according to the NL EQ-5D (95% confidence interval (CI) 0.016–0.189).
The QALYs during the entire follow-up period of 1 year as measured by the VAS, the valuation by the patients themselves, were significantly lower for PLDD patients (p¼0.02).
Healthcare costs
The average costs of initial PLDD treatment were E2751 lower (95% CI E2414 to E3088) than the average
costs of surgery, including the initial hospital admission of on average 3.0 days (Table 2).
Part of this difference in costs is compensated by a higher rate of reoperations (44% for PLDD versus 16%
for conventional discectomy). As a result, the costs per patient of the reoperations (conventional discectomy)
were significantly higher for PLDD patients (average difference E1643, 95% CI E780 to E2506).
Over the first year, total healthcare costs for PLDD were significantly lower than conventional microdiscectomy,
with a difference in cost of E1771 (E303 to E3238) per patient.
Societal costs
The total non-healthcare costs after PLDD were lower than after conventional microdiscectomy with a nonsignificant difference of E609 (_E3840 to E5058). As the non-healthcare cost per patient is about twice the healthcare cost per patient, the significant difference in healthcare cost is not reflected in the societal costs, which is the sum of the healthcare and non-healthcare cost. The difference in total societal cost amounts to E2379 (_E2860 to E7618) per patient, non-significantly in favor of PLDD.
Cost utility analysis
The combination of lower societal costs and less favorable QALY outcomes makes the probability that
PLDD is cost-effective compared with surgery dependent on the willingness to pay: if a society is only willing
to pay a small amount for a QALY, the lower societal costs of PLDD will outweigh the monetary value of the
less favorable QALY outcomes. This is shown in Figure 1: for low values of the willingness to pay for
a QALY, the probability that PLDD is cost-effective compared with conventional microdiscectomy is higher
than 0.5. For higher values of the willingness to pay, the monetary value of the QALY-loss, as result of PLDD, will be higher than the savings in societal costs of PLDD. This means that surgery becomes favorable
and the probability of PLDD being cost-effective is in Figure 1 decreasing below 0.5.
In the base case analysis, using the US EQ-5D and the societal perspective, PLDD was more likely to be
cost-effective than surgery for a willingness to pay of E70,000 per QALY and lower. From the healthcare
perspective, PLDD was more likely to be cost-effective for a willingness to pay of E50,000 and lower.
According the NL EQ-5D, PLDD was more likely to be preferred for a willingness to pay below E40,000 and
E30,000, for the societal and the healthcare perspective respectively (Figure 1).
Table 1. Utility and QALYs after PLDD or conventional microdiscectomy.
Values are means (standard deviations)
Discussion
Although, for higher values of willingness to pay, surgery becomes more likely to be cost-effective, the acceptability curves in this randomized study show that, for low values of the willingness to pay, PLDD is more likely to be cost-effective. The results show that at internationally used threshold values, of the willingness to pay per QALY, there is indifference between both methods from a societal perspective. In that case, treatment can be based on patient preference.
This makes PLDD a viable nonsurgical treatment option for patients with sciatica, caused by small and contained herniated discs, who do want to postpone the decision for surgery.
The EQ-5D and SF-6D results showed that utilities for PLDD were less favorable than for conventional surgery (especially in the second quarter), but over the entire year the difference in QALYs was not significant.
This was in accordance with the results of the Roland Disability Questionnaire which were not significantly different at 1 year. Also the perceived recovery and the VAS scores for leg and back pain at 52 weeks did not differ significantly. However, a significant difference in the improvement of the VAS score for leg pain and speed of recovery was observed during the first year, in favor of conventional microdiscectomy.
The expected lower costs of PLDD were confirmed: average costs of PLDD treatment were E2751 lower compared with microdiscectomy. Based on the differences in personnel, consumables, operation room time, anesthesia and shorter hospitalization, we assume that this difference is not only applicable to the NL but also holds in the other European countries and US. This difference in average costs was significant and even though the reoperation rate was considerably higher in the PLDD group (44% versus 16%), total healthcare costs after PLDD remained significantly lower than conventional microdiscectomy, with a difference in cost of E1771 per patient.
Also, non-health care costs were lower for PLDD patients in comparison with patients that underwent surgery, mainly due to lower absenteeism in the first quarter in the PLDD group, but this difference was not statistically significant. In total this resulted in a non-significant difference in societal costs of E2379 per patient in favor of the PLDD group. The acceptability curves show that if society is only willing to pay a low price for a QALY, PLDD is more likely to be cost-effective (value higher than 0.5 in Figure 1).
For higher values of the willingness to pay, between E30,000 and E70,000, this probability decreases below 50% (lower than 0.5 in Figure 1) in which case conventional microdiscectomy becomes more likely to be cost-effective. The internationally accepted threshold values per QALY of E40,000 in the Netherlands11,12 and US$50,000 in the US lie well within the mentioned range of E30,000 to E70,000, which indicates that from an economic viewpoint there is no preference for PLDD or conventional surgery.
In an earlier study on the Sciatica Trial, our group compared surgery with prolonged conservative care. This study resulted in the conclusion that surgery was likely to be cost-effective compared with prolonged conservative care, due to a significant gain in QALYs at comparable costs. The savings on costs of surgery after prolonged conservative care were balanced mainly by lower productivity costs after microdiscectomy. In our current study the effects on medical and non-medical costs were not in opposite directions: both treatment costs and productivity costs were lower for PLDD than for microdiscectomy. However, our current study was confined to small and contained disc herniations, whereas in the Sciatica Trial no restriction was made regarding the size of the herniation. Due to these differences a direct comparison cannot be made.
Nevertheless, the fact that our PLDD patients were already surgical candidates and therefore a different
subgroup, can be used to argue that there may be a role for PLDD in the general population that is considered for conservative therapy in order to avoid surgery. Hence, a direct evaluation of PLDD compared
with prolonged conservative care should be performed to evaluate the role of PLDD as an adjunct to onservative care and also the role in the treatment of larger disc herniations.
This study has several limitations. Firstly, patients were aware of which randomization group they were
in, so their reported utilities and costs may have been influenced by their preference for treatment. One
third of the patients stated to have no preference for treatment, 24% preferred conventional treatment
and 42% preferred PLDD. If this difference in preference would have influenced the results, it would also have biased the results towards a more positive outcome in favor of PLDD. Preliminary analysis did however not show that patient preference had a statistically significant effect on the outcome.
Furthermore, patients with a preference for PLDD may still have undergone surgical decompression and vice versa.
Secondly, the duration of the economic evaluation was limited to 1 year; however, the differences in utility values and costs between the groups decreased to slight differences in the last quarter, indicating that the most important effects are included in the 1-year study period. The outcomes in ‘patient perceived recovery
at 2 years14 are of interest, however, and may also impact the treatment decision. This is the case since at 2 years the PLDD group had 71% perceived recovery versus 61% in the surgery group (odds ratio (OR) 1.6, 95% CI 0.7–3.6) whereas at 1 year the PLDD group had a lower perceived recovery than the surgical group being 69% versus 75% respectively (OR 0.81, 95% CI 0.4–1.9).
Thirdly, an important drawback of the study, is the fact that the disc herniations of larger sizes were randomized in the parallel sciatica micro-tubular discectomy study15 and only those with a smaller disc herniation and longer duration were included in this PLDD study.
Table 2. Mean healthcare costs and societal cost per patient after PLDD or conventional microdiscectomy. Volumes are percentages of patients that made costs for that item, unless stated otherwise.
DOWNLOAD TABLE 2 IN PDF
There is often doubt regarding the decision to perform surgery in the smaller disc herniations and long standing complaints. This might also be the cause for the worse results in this patient population compared with the population of the Sciatica Trial by the same research group.
Finally, the analysis is performed in a Dutch context, which may not be representative for other settings. In other situations, with for example lower reoperation percentages or lower hospital durations for microdiscectomy, or higher costs of PLDD, microdiscectomy will be the preferred treatment, and vice versa.
In other settings, the costs may be higher but this is unlikely to reverse the cost difference.
In conclusion, a strategy using PLDD as the primary treatment for sciatica, followed by surgery when needed, appears to be an economically neutral innovation for smaller disc herniations. This makes PLDD an interesting nonsurgical treatment option for patients who do want to postpone the decision for surgery.
A study, comparing a strategy of PLDD as a minimally invasive intervention with conservative ‘watchful waiting’, including those patients with larger disc herniations, is warranted.
Acknowledgments
Role of the Sponsor: The Dutch Health Care Insurance Board did not participate in the design and conduct of the study, in the collection, analysis, and interpretation of the data, or in the preparation, review, or approval of the manuscript.
Enrolling physicians and treating neurosurgeons: WF Tan, R Brouwer (Medical Center Alkmaar) F Kloet, R Walchenbach, H Wurzer, M Arts, W Peul (Medical Center Haaglanden), R Kuiters, C Hoffmann, (Haga Hospital, The Hague), T Menovsky (UMC Nijmegen) A Dallenga (St. Franciscus Hospital, Schiedam) and A Vincent PLDD-physicians: G Lycklama a Nijeholt, B van der Kallen, A Bot, M van Proosdij, T van der Vliet, PA Brouwer and B Schenk.
Research-nurses and members of the SIPS-team: L Smakman, G Holtkamp, P Bergman, S Dukker, J Videler, A Mast, M Nuyten, M van Iersel, M Oosterhuis, M Scholten, A Nieborg, G Labadie and C Waanders.
Declaration of conflicting interests The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article. This study was funded by the Dutch Health Care Insurance Board.
References
INR Interventional Neuroradiology
2017, Vol. 23(5) 538–545
|
 Facebook
Facebook